Do you lie awake at night, staring at the ceiling? You’re not alone. Millions of Americans face sleep difficulties that mess with their lives. Whether it’s sleep problems now and then or insomnia all the time, knowing what’s going on is the first step.
Poor sleep does more than just make you tired. It can hurt your brain, weaken your immune system, and even raise your risk for big health problems like heart disease and depression. But, many sleep problems have clear causes that can be fixed.
Today, we have many ways to get better sleep. There’s therapy for insomnia, changes in how we live, and even medicine. This guide will help you understand your sleep issues and find the best way to fix them.
Key Takeaways
- Chronic sleeplessness affects millions of Americans and can lead to serious health complications
- Sleep disorders have distinct patterns, causes, and treatments that require different approaches
- Cognitive Behavioral Therapy for Insomnia (CBT-I) is considered the first-line treatment for chronic sleep problems
- Lifestyle factors including diet, exercise, and bedroom environment significantly impact sleep quality
- Understanding the underlying causes of your sleep difficulties is essential for effective treatment
- Both medical interventions and natural remedies can be effective, depending on your specific situation
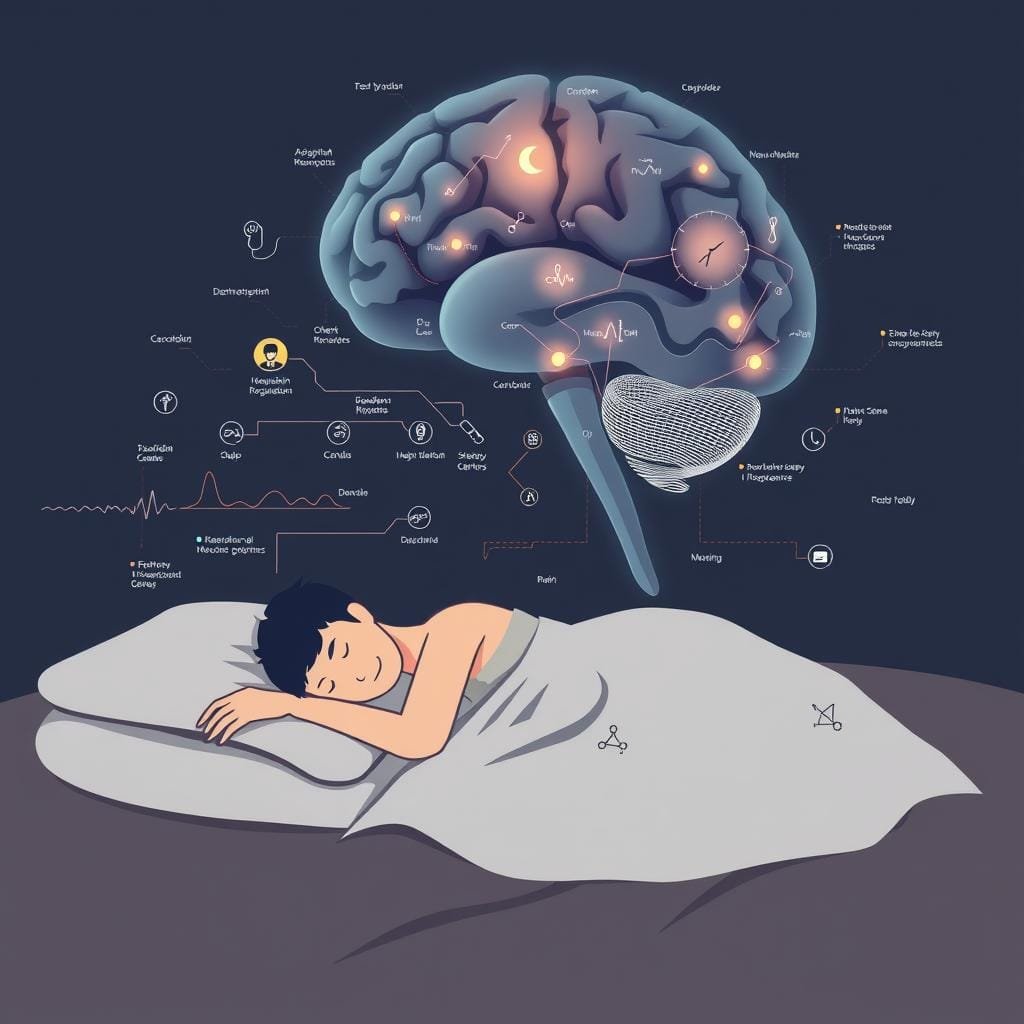
The Science Behind Sleep and Wakefulness
Sleep and wake cycles are amazing. They are controlled by hormones and brain activity. Our bodies get tired and wake up in a cycle every 24 hours.
Sleep is not just being asleep. It’s when our brain works hard. It needs balance to sleep well.
Normal Sleep Cycles and Architecture
At night, we go through different sleep stages. Each stage is special and lasts about 90-110 minutes. This is called sleep architecture.
First, we sleep lightly. Then, we sleep deeply. This is when our body fixes itself and remembers things. REM sleep is when we dream. It helps us feel and think better.
Our circadian rhythm controls these sleep cycles. It’s like a 24-hour clock in our body. It tells us when to sleep and wake up.
How Sleep Needs Change Throughout Life
How much sleep we need changes as we get older. Babies sleep a lot. Older people sleep less and not as deeply.
| Age Group | Recommended Hours | Sleep Characteristics | Common Challenges |
|---|---|---|---|
| Newborns (0-3 months) | 14-17 hours | Multiple sleep periods throughout day/night | No established circadian rhythm |
| Children (6-12 years) | 9-12 hours | Consolidated nighttime sleep | Resistance to bedtime |
| Teenagers (13-17 years) | 8-10 hours | Delayed sleep phase | Difficulty falling asleep early |
| Adults (18-64 years) | 7-9 hours | Stable sleep patterns | Work/life stress disrupting sleep |
| Older Adults (65+ years) | 7-8 hours | Earlier bedtimes, earlier waking | More nighttime awakenings |
Teenagers feel more awake at night. They sleep in later. This is why school starts too early for them.
Older adults sleep less deeply. They wake up more at night. This makes them feel tired even when they sleep enough.
Knowing how sleep changes with age helps us understand sleep problems. It’s important to know what our body needs based on our age.
Defining Sleeplessness: Types and Classifications
Not all sleep problems are the same. Knowing the type you have is key to getting better. Sleep issues range from occasional bad nights to long-term insomnia that affects daily life. Knowing this helps you talk to doctors and find the right help.
Insomnia vs. Occasional Sleep Difficulties
Everyone has bad sleep nights sometimes. This can be due to stress, travel, or changes in the environment. Insomnia, on the other hand, is a serious condition with clear signs.
Insomnia makes it hard to fall or stay asleep. It lasts for at least three months and makes daily life hard. It’s not just about having a bad night.
Knowing the difference is important. Simple changes can fix occasional sleep issues. But insomnia needs more help. If sleep problems affect your day, see a doctor.
Onset, Maintenance, and Early-Morning Awakening Insomnia
Insomnia can start in different ways. Sleep onset insomnia is when it’s hard to start sleeping. It’s often due to worries or body clocks that are off.
Sleep maintenance insomnia is when you wake up a lot during the night. People with this feel frustrated and can’t sleep. It’s linked to pain, sleep apnea, or stress.
Early-morning awakening insomnia is when you wake up too early. It’s common in depression and as people get older. Many people have more than one type, which can change over time.
Acute vs. Chronic Sleeplessness
How long you have sleep problems matters. Acute insomnia is short-term, lasting less than three months. It’s often caused by big stressors like job loss or health issues. It usually gets better once the stress goes away.
Chronic insomnia lasts more than three months. It affects about 10-15% of adults. It’s caused by many things, including biology, psychology, and environment. The longer it lasts, the harder it is to break the cycle.
Knowing if your sleep problem is short-term or long-term helps find the right treatment. Short-term insomnia might need just a little help. But long-term insomnia needs a bigger plan to fix it.
The Physical and Mental Impact of Sleep Deprivation
Chronic sleep deprivation is a silent health saboteur. It slowly harms mental and physical health. Many people don’t see these effects. But, it’s important to understand them to fight sleep problems.
Cognitive and Emotional Effects
Sleep loss hurts your brain in many ways. It makes it hard to do simple tasks. Just one bad night of sleep can make you feel like you’re drunk.
Your memory and learning suffer without enough sleep. Your brain needs sleep to keep memories and learn new things. Without it, you can’t remember well and learn slowly.
When you’re tired, you make bad choices. You take risks, can’t think creatively, and make poor decisions. You also have trouble adapting to new situations.
Sleep loss also affects your mood. It makes you irritable and moody. Without sleep, your brain can’t handle emotions well. This leads to more anxiety and depression.
Long-term Health Consequences
Chronic sleep loss leads to serious health problems. Your body needs sleep to work right. Without it, your body’s systems start to fail.
Poor sleep causes inflammation in your body. This inflammation can lead to many serious diseases. Sleep loss is not just about feeling tired; it can change how your body works and make you sick.
Cardiovascular Risks
Not enough sleep raises your heart risks. It makes your blood pressure and heart rate go up. This can lead to heart disease and stroke.
Poor sleep also hurts your heart health. This creates a cycle that’s hard to break. You need to work on both sleep and heart health.
Metabolic Disruptions
Sleep loss messes with how your body handles sugar and hunger. It can make you insulin resistant, like a pre-diabetic. It also messes with hormones that control hunger.
This is why sleep loss is linked to weight gain and diabetes. It also makes you less active, making things worse.
Immune System Impairment
Your immune system needs sleep to fight off infections. Without enough sleep, your body can’t make the proteins it needs to fight off sickness. This makes you more likely to get sick and take longer to get better.
Chronic sleep loss also weakens your immune system. It increases your risk of autoimmune diseases and makes vaccines less effective. Sleep is key to keeping your immune system strong.
Medical Causes of Sleeplessness
Many Americans struggle with sleep because of health issues. These problems can make it hard to sleep well. Finding out what’s causing your sleep trouble is key to feeling better.
Primary Sleep Disorders
Primary sleep disorders are big problems on their own. They mess with how we sleep and can really hurt our lives.About 50-70 million US adults deal with these issues, leading to a lot of sleep trouble.
Sleep Apnea
Sleep apnea means you stop breathing a lot while you sleep. This makes it hard to get good rest. It’s caused by the airway getting blocked or brain signals going wrong.
Restless legs syndrome makes you want to move your legs a lot at night. It’s a brain problem that feels like tingling or aching. It affects 7-10% of Americans and can make it hard to fall asleep.
Circadian Rhythm Disorders
Circadian rhythm disorders mess up your body’s clock. They make it hard to sleep at the right times. This can happen to night owls, early birds, or people who work shifts.
Other Medical Conditions
Many health problems can mess with your sleep. Conditions like arthritis make it hard to find a comfy sleeping spot. Breathing issues like asthma can wake you up at night.
Stomach problems like acid reflux can also keep you awake. Neurological issues like Parkinson’s disease can cause pain and movement problems that disrupt sleep.
Hormonal imbalances can also affect sleep. Problems like thyroid issues, menopause, and diabetes can lead to night sweats or needing to get up a lot. Heart problems can make it hard to breathe when lying down, making sleep even harder.
| Medical Condition | Sleep Symptoms | Mechanism | Treatment Approach |
|---|---|---|---|
| Chronic Pain | Difficulty falling/staying asleep | Physical discomfort | Pain management, sleep positioning |
| Acid Reflux | Nighttime awakenings | Stomach acid irritation | Dietary changes, elevated head position |
| Hyperthyroidism | Insomnia, restlessness | Metabolic overactivity | Thyroid medication, stress reduction |
| Heart Failure | Orthopnea, sleep apnea | Fluid accumulation in lungs | Cardiac treatment, elevated sleeping position |
Medication Side Effects and Interactions
Many medicines can mess with your sleep. Drugs for ADHD, asthma, and colds can keep you awake. Some antidepressants might make sleep worse at first.
Medicines for high blood pressure can mess with melatonin, affecting sleep. Steroids for inflammation can make you feel more awake. Even pain relievers with caffeine can disrupt sleep.
When medicines mix, they can have bad effects on sleep. Always talk to your doctor if you’re having sleep problems. Changing your medicine or when you take it might help without hurting your treatment.
Psychological Factors Contributing to Sleeplessness
Our minds and feelings also affect how well we sleep. Medical issues can mess with our sleep, but our thoughts and feelings can too. Knowing what our minds do to our sleep is key to fixing it.
Stress, Anxiety, and Hyperarousal
Stress and sleep are linked in a bad way. Stress makes our body ready to run or fight. This is the opposite of what we need to sleep.
Anxiety insomnia happens when we worry too much at night. Our minds stay awake, making it hard to sleep. This keeps us awake and worried.
For those with sleep anxiety, bed becomes a source of stress. The fear of not sleeping well makes it hard to sleep.
Depression and Other Mood Disorders
Depression sleep problems are a two-way street. Depression can mess with our sleep, and not sleeping well can make depression worse. This makes it hard to break the cycle.
Bipolar disorder also affects sleep. Manic phases make us need less sleep, while depressive phases make it hard to sleep. PTSD can also mess with our sleep, causing nightmares and keeping us awake.
Fixing mood disorders can help us sleep better. And fixing sleep problems can also help our mood. This shows how connected these issues are.
Cognitive Patterns That Disrupt Sleep
People with sleep problems often think in ways that make it worse. Racing thoughts at night is a big problem for many.
Some common thoughts that mess with sleep are:
- Catastrophizing about the consequences of poor sleep (“I’ll be completely useless tomorrow”)
- Rumination over past events or future worries
- Unrealistic expectations about how quickly one should fall asleep
- Performance anxiety about sleep itself (“I must get 8 hours or else”)
These thoughts make it hard to relax and fall asleep. Therapy for insomnia helps change these thoughts to help us sleep better.
Diagnosing the Root Causes of Sleeplessness

Finding out why you can’t sleep well needs special tests. These tests look at how your body works and how you act. Getting a sleep diagnosis is key to fixing your sleep problems. Doctors and sleep tracking help find what’s wrong.
Medical Evaluations and Sleep Studies
Starting to fix your sleep often means talking to a doctor. They’ll look at your health history and what you’re taking. They might also check for physical things that could mess with your sleep.
If your sleep problems don’t go away, you might see a sleep expert. They use special tests to see how tired you are. This helps them understand how bad your sleep problems are.
For harder cases, a polysomnography (sleep study) might be needed. This test watches your body while you sleep. It looks at things like your brain waves and how you breathe.
This test can find sleep disorders like sleep apnea. It helps figure out why you can’t sleep well.
Self-Assessment Tools and Sleep Tracking
Watching yourself can also help find sleep problems. Keeping track of your sleep can show patterns. This might not show up in just one doctor visit.
Sleep Diaries and Journals
A sleep diary is a great tool for tracking your sleep. Writing down your sleep for a week or two helps a lot. It shows how long it takes to fall asleep and how often you wake up.
Also, write down things that might mess with your sleep. This could be caffeine, exercise, or stress. These things can affect how well you sleep.
Technology-Based Sleep Monitoring
Today, there are easy ways to track your sleep. Wearable devices and apps can monitor your sleep. They can tell how long you sleep and even what stage you’re in.
Smartphone apps can also track your sleep. They can wake you up when you’re in a light sleep phase. Bedside monitors can track your sleep without touching you.
While these tools aren’t as precise as sleep studies, they’re helpful. They give you and your doctor clues to fix your sleep problems.
Evidence-Based Medical Treatments for Sleeplessness
Modern sleep medicine offers many treatments to help with sleep problems. These treatments can help when natural methods don’t work. The right treatment depends on the cause of sleeplessness, how long it lasts, and your health.
Prescription Sleep Medications
Prescription sleep medicines can be helpful short-term solutions for insomnia. They work in different ways to help you sleep.
Benzodiazepines and Non-Benzodiazepine Hypnotics
Benzodiazepines like temazepam and “Z-drugs” (zolpidem, zaleplon, eszopiclone) help by affecting GABA in the brain. They’re good for short-term insomnia but can lead to dependence and next-day effects.
Melatonin Receptor Agonists
Medicines like ramelteon act like melatonin, the body’s sleep hormone. They don’t cause dependence or withdrawal. They’re great for people with delayed sleep phase syndrome or disrupted circadian rhythms.
Newer medicines like suvorexant and lemborexant block orexin, a wakefulness neurotransmitter. They help you fall asleep faster and stay asleep longer. They have fewer side effects than older medicines.
| Medication Type | Examples | Mechanism | Best For | Considerations |
|---|---|---|---|---|
| Benzodiazepines | Temazepam, Triazolam | Enhances GABA effects | Short-term sleep onset issues | Risk of dependence, rebound insomnia |
| Z-drugs | Zolpidem, Zaleplon | Selective GABA modulation | Sleep onset difficulties | Less residual daytime sedation |
| Melatonin Agonists | Ramelteon | Activates melatonin receptors | Circadian rhythm disorders | No dependence risk, fewer side effects |
| Orexin Antagonists | Suvorexant, Lemborexant | Blocks wake-promoting signals | Sleep maintenance insomnia | Newer option, preserves sleep architecture |
Cognitive Behavioral Therapy for Insomnia (CBT-I)
CBT-I is the top choice for chronic insomnia. It changes thoughts and behaviors that cause sleep problems. Research shows CBT-I works as well or better than sleep medicines for long-term insomnia.
A CBT-I program includes several parts:
- Sleep restriction therapy – Limits time in bed to improve sleep efficiency
- Stimulus control – Helps break bad sleep associations
- Cognitive restructuring – Changes negative sleep thoughts
- Relaxation techniques – Reduces tension and mental arousal
- Sleep hygiene education – Teaches sleep-promoting behaviors
CBT-I needs 6-8 sessions with a therapist. Digital CBT-I programs are also effective. CBT-I’s effects last long after treatment ends, making it a lasting solution.
Other Therapeutic Approaches
There are other treatments for sleep disorders:
Light therapy uses bright light to reset the body’s clock. It’s great for circadian rhythm disorders and seasonal affective disorder.
Continuous positive airway pressure (CPAP) therapy keeps airways open during sleep. It treats obstructive sleep apnea that causes frequent awakenings.
Mindfulness-based therapy for insomnia combines meditation with CBT-I. Early studies show it can reduce stress and improve sleep, helping those with insomnia linked to anxiety.
Finding the right treatment plan is key. The best plans mix different treatments based on your sleep issues, health, and preferences.
Natural Remedies and Lifestyle Strategies for Better Sleep
Natural ways to improve sleep are gentle and effective. They can help with sleep problems or work with medicine. Many people mix different methods to make a sleep routine that works for them.
Using these methods regularly can make sleep better and improve health.
Evidence-Based Supplements and Herbal Remedies
Some natural supplements help with sleep, studies show. Melatonin supplements are well-studied. They help with sleep problems, like jet lag. Take 0.5-5mg 30-60 minutes before bed.
Valerian root might help sleep a bit. Magnesium can ease restless legs and muscle tension at night. L-theanine in tea relaxes without making you sleepy.
Always talk to a doctor before trying supplements. This is true if you’re on medicine or have health issues. Natural doesn’t mean safe, and quality can vary.
| Supplement | Typical Dosage | Best For | Potential Side Effects |
|---|---|---|---|
| Melatonin | 0.5-5mg | Jet lag, delayed sleep phase | Morning grogginess, headaches |
| Valerian Root | 300-600mg | General sleep quality | Headaches, digestive upset |
| Magnesium | 200-400mg | Muscle tension, restlessness | Digestive issues in high doses |
| L-theanine | 200-400mg | Anxiety-related sleep problems | Minimal reported side effects |
Sleep Hygiene Best Practices
Sleep hygiene means good sleep habits. Go to bed and wake up at the same time every day. This helps your body get into a rhythm.
Do something relaxing before bed, like reading or meditation. Don’t look at screens for 30-60 minutes before bed. Blue light can mess with your sleep.
Make your bedroom just for sleep and love. If you can’t sleep, get out of bed and do something calm until you’re tired.
Daytime habits affect sleep too. Don’t drink caffeine after noon or alcohol close to bedtime. It can mess with your sleep. Morning sunlight helps keep your body clock in check.
Diet, Exercise, and Environmental Factors
What you eat, how you move, and where you sleep all affect sleep. Making smart changes in these areas can help without medicine.
Nutrition for Sleep
Some foods help sleep because of their nutrients. Turkey, eggs, and cheese have tryptophan for serotonin and melatonin. Whole grains, nuts, and bananas with potassium help relax muscles and regulate sleep.
Physical Activity Timing
Exercise is good for sleep, but when you do it matters. Morning or afternoon workouts are best. Evening workouts can keep you awake. Aim for 30 minutes of light activity daily, 3+ hours before bed.
Bedroom Environment Optimization
Make your bedroom a sleep haven. Keep it cool (65-68°F/18-20°C) and quiet. Use earplugs or white noise. Make it dark with curtains or an eye mask. Choose a good mattress and pillows for your sleep style.
Taking Control of Your Sleep Health: Next Steps and Resources
Now that you know about sleep disorders, it’s time to act. If simple sleep tips don’t work, see a sleep specialist. They are key when sleep problems last too long.
Start by talking to your doctor. They can send you to sleep centers. The American Academy of Sleep Medicine has a list of places with experts. Veterans can use a self-help workbook and app from the VA.
Before your visit, keep a sleep diary for two weeks. Write down when you go to bed and wake up. Also, note any sleep problems. This helps doctors find what’s wrong.
Online help for insomnia is growing. You can get help from home. Many insurances cover these online visits.
Good treatment might include therapy, lifestyle changes, and sometimes medicine. Getting better sleep takes time and effort. But with the right help, you can sleep better and feel better too.
